New Study Shows Regional Differences in Improved Survival of Patients with De Novo Metastatic Breast Cancer Over Time
In 2014, one year after its formation, the Metastatic Breast Cancer Alliance (MBC Alliance) published Changing the Landscape for People Living with Metastatic Breast Cancer. Chapter 5 of the analysis showed a lack of data about the population of metastatic breast cancer (MBC) patients living across the US. The MBC Alliance identified key questions to be answered about MBC epidemiology in the areas of incidence, prevalence, and outcomes, and how these changed over time.
The newly published study by Malmgren et al. is the fourth in a series of articles published on aspects of this topic.
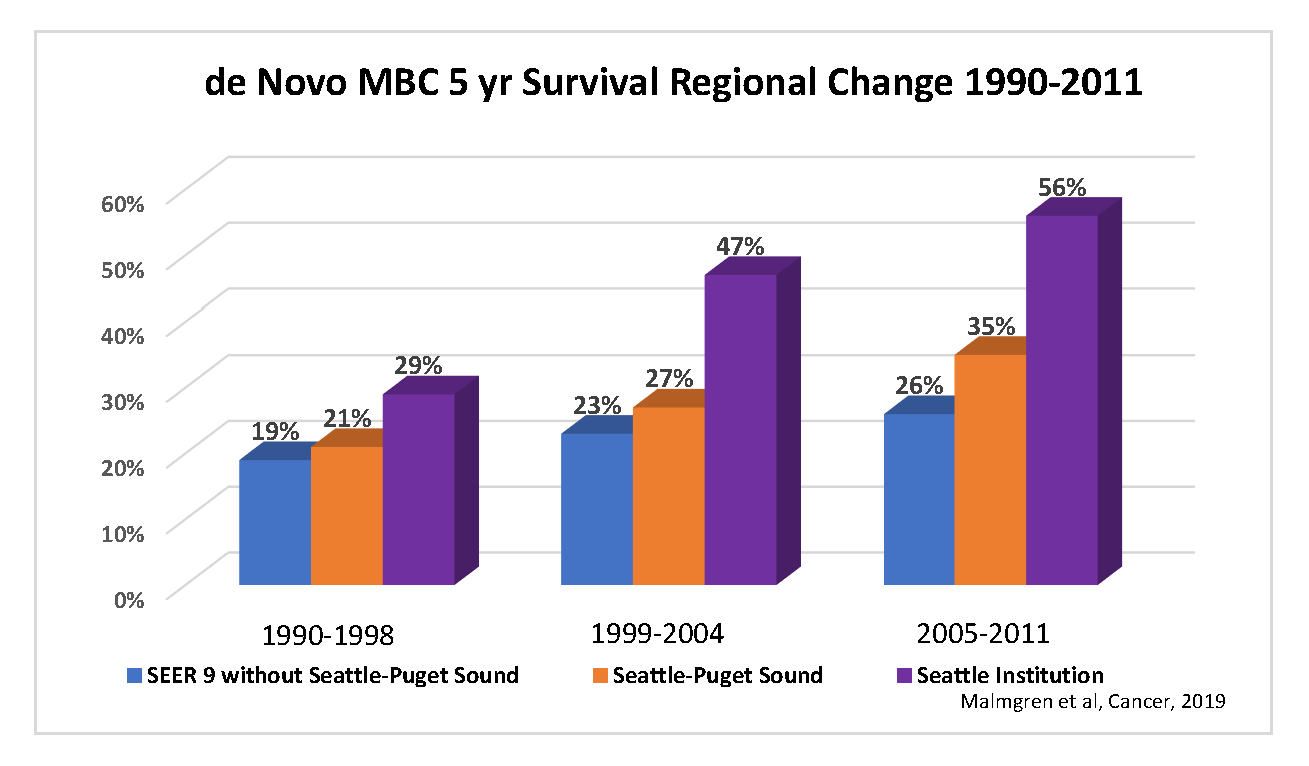
The newly published article looked at regional differences in survival in patients with de novo MBC (dnMBC), which is a first diagnosis of breast cancer that is stage IV. The authors studied dnMBC patients in the Surveillance, Epidemiology, and End Results (SEER) 9 registry, which includes cancer patients living in nine regions of the US: Connecticut, Detroit, Atlanta, San Francisco-Oakland, Hawaii, Iowa, New Mexico, Seattle-Puget Sound, and Utah. They also studied an institutional cohort, which is a group of breast cancer patients living in the Seattle area whose data are recorded in a longitudinal database. In a longitudinal database, data for patients are updated over time as the patients continue to receive care. These patients live in the Seattle-Puget Sound registry area and are included in SEER Seattle-Puget Sound. They compared 5-year breast cancer-specific survival in dnMBC patients in SEER 9 without Seattle-Puget Sound, SEER Seattle-Puget Sound only, and the institutional cohort.
- They found that between 1990 and 2011, breast cancer-specific survival for dnMBC patients improved over time and increased from 19% to 26% in SEER 9 without Seattle-Puget Sound, from 21% to 35% in SEER Seattle-Puget Sound only, and from 29% to 56% in the institutional cohort. Thus, 5-year survival with dnMBC is different depending on where the patients lived.
- Survival also improved as new treatments were introduced. In the institutional cohort, surgery, initial chemotherapy, a diagnosis between 2005 and 2011, and younger age were associated with better survival. Surgery, a diagnosis between 2005 and 2011, younger age, and region of residence were important factors associated with survival in SEER 9.
Given the increase in survival for dnMBC, aggressive treatment that is intelligent, evidence based, timely, and receptor subtype-specific appears to have substantially extended the lives of these MBC patients. The observations suggested that patients should be offered subtype-appropriate care, such as hormone therapy for hormone receptor-positive patients not suffering from visceral crisis and trastuzumab-based therapies for HER2-positive patients. These and other treatments may allow dnMBC patients to experience more important events in their life (weddings, graduations, etc.), and dnMBC patients with oligometastases (one or few metastatic sites) are especially likely to benefit from such an approach.
Earlier MBC epidemiology studies performed in partnership with the MBC Alliance included:
The first article in this series focused on the population across the US and estimated the number of people living with MBC. This study was done in partnership with the NCI SEER database statistical experts. The study authors found that about 155,000 people in the US are living with MBC.
The next article investigated key MBC epidemiology questions in more detail. The MBC Alliance and collaborators worked with a hospital that had a longitudinal database containing a large number of cases with long-term follow-up. The key questions pertained to incidence as well as outcomes in survival for recurrent MBC (rMBC) compared to dnMBC. The SEER database is not suitable for such a study because it only captures dnMBC and not rMBC. For this study, the authors examined the long-term institutional cohort described above. These patients have been followed from 1990 through the present day. This study found that women with dnMBC had a 5-year survival rate of 44% compared to 20% of women with rMBC. Over the 20-year period, dnMBC 5-year survival improved by 27%, from 28% to 55%, but rMBC survival decreased over time.
The third article also investigated data from the institutional cohort in Seattle. They studied over 8,000 women with stage I-III invasive breast cancer, 11.6% of whom were later diagnosed with rMBC. The authors found a significant decline in rMBC over time, but no increase in survival. They also looked at receptor subtypes in detail. The incidence of HER2-positive and hormone receptor-positive rMBC decreased, but the incidence of triple negative (HER2 negative and hormone receptor negative) rMBC did not, creating a relative increase in triple negative rMBC overall.
The MBC Alliance and collaborators are continuing their efforts to understand the epidemiology of MBC. Data from previous, current, and future efforts will allow the MBC Alliance to develop policy messaging to better advocate for people living with MBC. Breast cancer organizations and advocates within the MBC Alliance are continuing their efforts to ensure that newly diagnosed MBC patients, no matter where they live in the US or what their socioeconomic background is, are knowledgeable about their cancer subtype; seek treatment from a healthcare team that uses evidence-based approaches to select the right treatment for them; and most importantly, have affordable access to the newest treatments for their disease.